Doulas Step Up to Comfort NYC Abortion Patients
By Molly M. Ginty
WeNews correspondent
Tuesday, August 31, 2010
 NEW YORK (WOMENSENEWS)--One woman was so nervous during her abortion that her sweat soaked through her paper gown.
NEW YORK (WOMENSENEWS)--One woman was so nervous during her abortion that her sweat soaked through her paper gown.A second apologized repeatedly for not being ready to have a child.
A third sobbed quietly because she was forced to terminate her pregnancy due to health complications.
During the two years that Lauren Mitchell has attended to the needs of women undergoing abortions, these three patients are among the hundreds she has served.
"Abortion is different for every woman, and though it can be straightforward and simple, it can in some cases be stressful," said Mitchell, co-founder of The Doula Project, a Manhattan-based nonprofit that trains volunteers to support women not only during delivery, but during abortions, too. "Regardless of the circumstances, we're here to help."
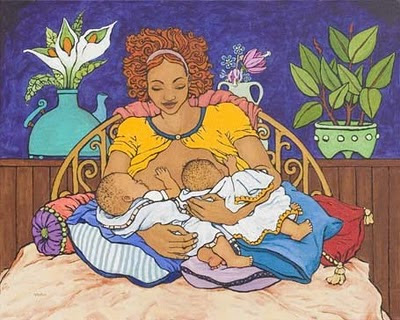
Doulas take their name from the Greek word for "caregiver." They typically help women through pregnancy and have become popular in recent decades as expectant mothers' birth plans have begun to include their services; some insurance providers have begun to cover those services, too.
A doula's work, for which she is usually compensated $25 to $35 per hour, ranges from providing parenting-book recommendations to offering guided relaxation and massage during labor. For the first weeks of a baby's life, she may also change diapers and perform housecleaning help.
In 2007, three New York City doulas--Mitchell and her colleagues Mary Mahoney and Miriam Pérez--decided to extend their services not just to women who complete pregnancies, but also to women who terminate them.
They partnered with two Manhattan abortion facilities in August 2008 and began training "abortion doulas" to work there free of charge.
Today, these 45 volunteers chat with patients in waiting rooms, hold their hands when they are on the operating table and provide them with warm blankets and hot water bottles that ease cramps during recovery.
Whether patients experience miscarriage, opt for medical abortion (mifepristone) at home or have the procedure at a clinic, they can decide to work with a doula or not.
Among the New York City women who have been offered this help--more than 1,500--all but one patient has accepted it, said Mitchell.
Replicating the Service
New York appears to be the only state where abortion doula services are available, but doulas in North Carolina and Washington State have their eyes on replicating the service."We weren't the first to come up with the idea that an abortion patient should be able to ask for this assistance," said Mitchell. "Nurses, escorts and counselors have long filled this role. But we decided to give it a name and to offer our services in a formal way because of the growing need for them."
Eighty-seven percent of U.S. counties have no abortion provider, and 35 percent of U.S. women live in those counties, reports the Guttmacher Institute, a health policy organization in New York City.
Due to this squeeze, some doctors perform 25 to 30 abortions per day, doing one every 20 minutes in an assembly-line fashion, with little time to chat or offer patients counseling and comfort, pro-choice advocates say.
Though abortion doulas provide support and assistance that is lacking, they take flak from both sides of the abortion divide for doing so. On one hand, they facilitate abortion, which sparks outrage from the anti-choice movement. On the other hand, their work acknowledges that terminating a pregnancy can be difficult, which some pro-choice supporters regard as a political Pandora's box.
On her blog, anti-choice activist Jill Stanek blasted abortion doulas for trying "to legitimize and de-stigmatize abortion by making it a component of maternity."
On the Web site AllDoulas.com, one anti-choice doula proclaimed, "I am an advocate for moms and babies, and aborting babies is totally opposite from that."
Pro-Choice Pushback Too
"We're also getting pushback from the pro-choice community," said Alison Ojanen-Goldsmith of Seattle's Full Spectrum Doulas, which is preparing to train abortion doulas this fall. "Some pro-choice advocates don't want to admit that abortion patients may need support. They deny it because they're fighting anti-choice rhetoric and its insistence that women are somehow damaged by abortion."On the progressive Web site Slate.com, one pro-choice journalist asked, "Are women really so fragile that they need a complete stranger to hold their hand at the doctor's?"
Mahoney, one of The Doula Project's co-founders, said the criticism doesn't interfere with her organization's work.
"This pushback isn't going to stop us from training abortion doulas across the U.S. And it won't distract us from offering our services to the women who need our help," she said.
A woman may want a doula's extra reassurance because she is a teenager who fears her parents' disapproval, or because she is a domestic violence survivor who is hiding her pregnancy from her abusive spouse. A patient may be upset because she is pregnant by a rapist, or mourning because she is pregnant by a man she loves and cannot afford to raise their child.
Some abortion patients do not tell their partners, friends or family members that they are terminating their pregnancies. Even if they do have someone to sit with them through the procedure, that person may not be permitted to do so.
"For security reasons, many clinics do not allow a patient to have a partner or friend with them," said Lauren Guy-McAlpin of the Spectrum Doula Collective in central North Carolina, which hopes to train abortion doulas within the next year.
Precautions Necessary
Security is so tight at the two Manhattan facilities that currently have abortion doulas that these clinics will not release their names in print. They have reason to take precautions. Since 1993, eight abortion clinic workers have been murdered by anti-choice extremists and since 1977 U.S. clinics have suffered more than 6,000 acts of violence, including bomb threats, arson and kidnappings, reports NARAL Pro-Choice America, based in Washington, D.C.Fear of clinic violence can heighten the anxiety that some patients already feel about having an abortion.
"On top of all this, there can be incredible shame and stigma surrounding abortion, even though this procedure is incredibly common," said Laura G. Duncan, a Brooklyn-based abortion doula. "Our job is to offer patients whatever they need: someone to joke with, someone to cry with, maybe someone to rub their feet."
Half of pregnancies in the United States are unintended, with 40 percent of those ending in abortion. Nearly half of U.S. women--43 percent--have an abortion by the time they are 45, reports the Pro-Choice Public Education Project, a nonprofit in New York City.
"Research indicates that though many women feel relieved following an abortion, 10 to 15 percent have some emotional difficulty afterward," said Ava Torre-Bueno, author of the book "Peace After Abortion" and a licensed social worker who counsels abortion patients in San Diego, Calif.
If patients want to talk after their procedures, abortion doulas may give them their own phone numbers, along with the number of an after-care abortion hotline run by Exhale, a nonprofit group in Oakland, Calif.
Remembering how an abortion doula helped her through a stillbirth two years ago, Rose Ferreira of New York City said, "It's incredible how her kindness made this bearable. She made me realize it was OK to feel frustration and anger at not being able to control this heartbreaking situation. Above all, she helped me feel strong and secure even though I was at first afraid."